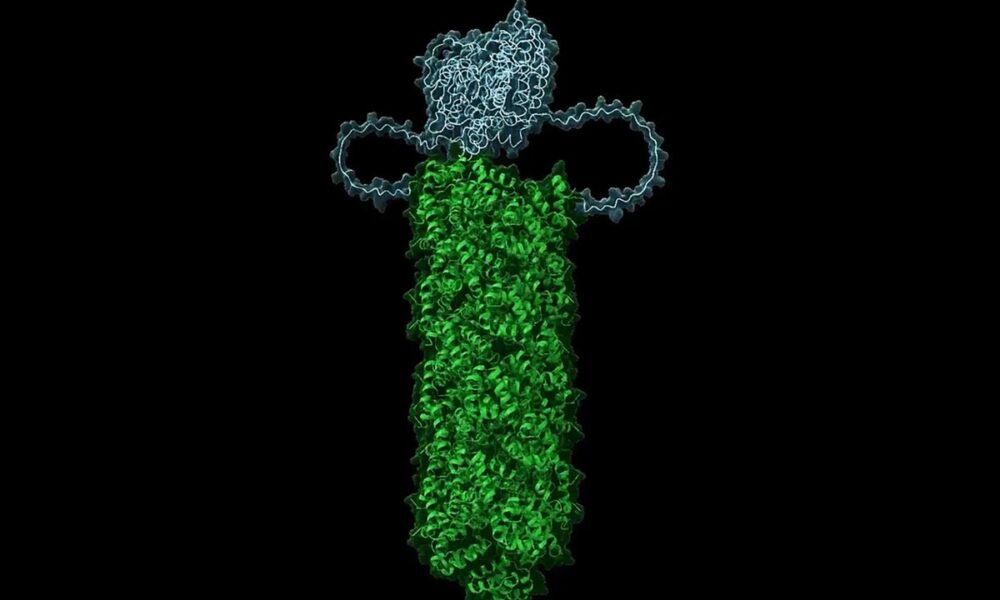
A recent study has revealed a novel mechanism by which human cells can trigger self-destruction in response to viral invasion. Researchers found that a specific group of approximately 100 immune proteins, which remain dormant within cells, can form a crystal structure when a virus penetrates. This structure facilitates the rapid activation of enzymes known as caspases, leading to a type of cell death termed pyroptosis.
The findings, published in the journal eLife in September 2023, detail how this mechanism operates as a swift response to viral threats, preventing potential spread throughout the body. According to Randal Halfmann, an associate investigator at the Stowers Institute for Medical Research, the cells are “literally waiting to die all the time.” This underscores the critical balance that immune cells must maintain between reacting to threats and avoiding unnecessary self-destruction.
Insights into Protein Behavior and Cell Decision-Making
Traditionally, scientists have focused on the individual structures of proteins to understand their functions. However, this research highlights a collective behavior among proteins that leads to significant cellular decisions. D. Allan Drummond, a molecular biologist at the University of Chicago, emphasized that an “explosion of discovery” is reshaping our understanding of how proteins interact and function together.
The study utilized living yeast cells and human cell lines to demonstrate that these immune proteins can crystallize over time, activating the cell death program. This rapid decision-making process is crucial, as reliance on slower signaling pathways could allow viruses to hijack the cell’s processes before a response is initiated.
Implications for Aging and Inflammation
Halfmann’s team quantified the crystallization driving force in various human cell types, discovering a correlation between protein concentration and the rate of cell turnover in the body. For instance, certain blood cells are replaced every few days, while neurons can last a lifetime. The higher concentration of these immune proteins in rapidly dividing cells suggests a link between spontaneous activation and cell death.
This mechanism may contribute to the low-grade inflammation often observed in aging. While strategies to prevent protein crystallization could extend cellular lifespan, Halfmann cautions that such interventions may weaken the immune response.
Moreover, this fundamental aspect of the immune system is not unique to humans; it is also present in early animal species, such as sponges, and even in bacteria. This aspect of self-sacrifice seems to have evolved as a community defense mechanism, where sacrificing one cell can protect related cells from viral threats.
The implications of this research extend beyond basic science. Understanding these protein interactions could lead to novel therapeutic approaches to manage inflammation and enhance immune responses. As the study progresses, it may open avenues for further exploration into how cells make critical life-or-death decisions and how these processes can be manipulated for better health outcomes.